Understanding Degenerative Disease
In the hands of reference mitral valve-repair surgeons, 95-100% of degenerative valves are repairable1,2, regardless of etiology; however, in the general cardiac surgical community, the repair rates are around 50%. In contrast to fibroelastic deficiency, Barlow's valves have more complex pathology and require advanced techniques to effect a repair.
Mitral valve regurgitation is present when the valve does not close completely, causing blood to leak back into the left atrium. Mitral valve stenosis is present when the valve does not open completely, causing a relative obstruction to blood flow. Both of these conditions increase the workload on the heart and are very serious conditions. If left untreated, they can lead to debilitating symptoms including cardiac arrhythmia, congestive heart failure, and irreversible heart damage.
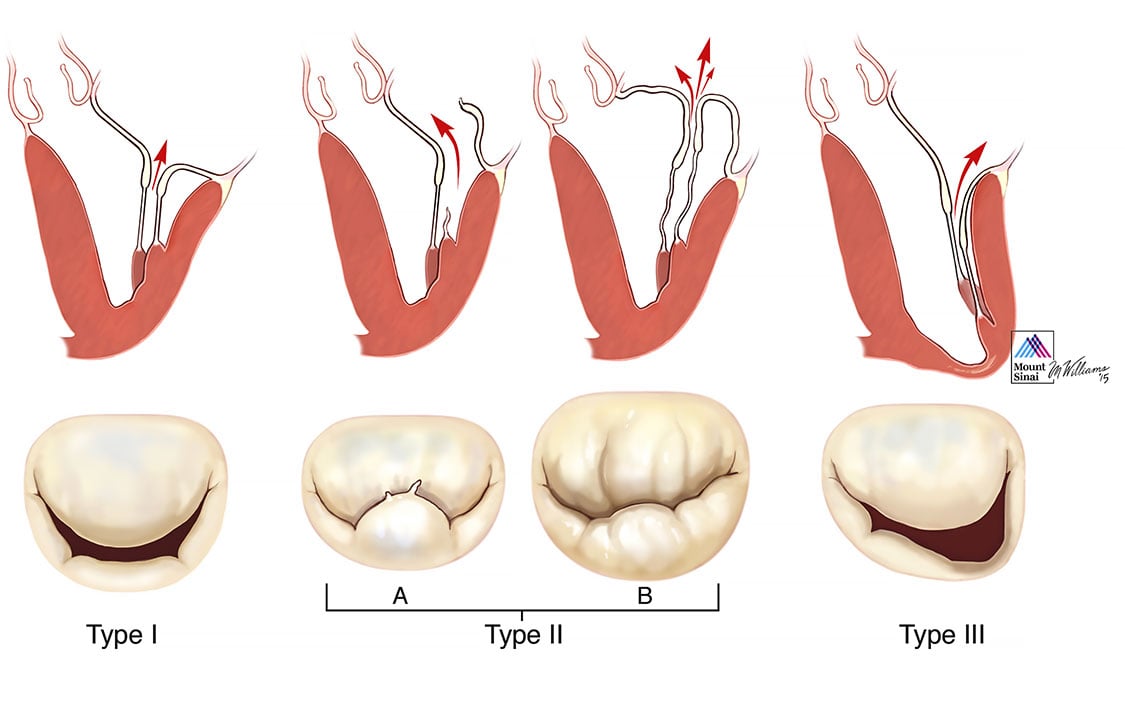
Carpentier refers to the confusion surrounding classification and description of mitral valve disease as “the Babel Syndrome,” in reference to the Biblical story of what happens when workers do not speak the same language3. Degenerative mitral valve disease is the best example of this phenomenon, where terms such as prolapse, flail, partial flail, billowing, Barlow’s disease, floppy valve, and myxomatous valve disease are often used inter-changeably by different specialists, blurring the distinction between valve dysfunction and disease. Carpentier’s pathophysiologic triad3 describes the inter-relationship between etiology (the cause of the disease), lesions (the result of the disease) and leaflet motion dysfunction (which results from the lesions). Carpentier’s classification of dysfunction is based on the opening and closing motions of the mitral leaflets in relation to the annular plane (Figure 1). It is in this context that degenerative mitral valve disease is best understood.
The most common leaflet dysfunction in degenerative valve disease is Type II, excess motion of the margin of the leaflet in relation to the annular plane. The lesions in degenerative valve disease that result in the Type II dysfunction are usually chordae elongation or rupture. Annular dilatation is almost always an associated finding. The most common diseases that cause degenerative mitral valve disease are Barlow’s disease and fibroelastic deficiency (Figure 2). Barlow’s disease, first described in the 1960s4, is characterized by several distinguishing features. Excess leaflet tissue with large billowing and thickened leaflets is a hallmark of Barlow’s disease, and the annular size is quite large. The chordae tendinae tend to be thickened and have a mesh type appearance in their insertion in the body of the leaflets. Chordal elongation is the most common cause of prolapse, and multiple leaflet segments are usually involved. It generally occurs in younger patients (aged <60 years), who have a long history of a heart murmur.
In contrast, fibroelastic deficiency is a degenerative disease of older individuals (usually >60 years of age), with a shorter history of valve regurgitation5. Rupture, often of a single chord, is the most common cause of leaflet dysfunction in fibroelastic deficiency, and in most cases the only abnormal leaflet tissue is found in the prolapsing segment. The other leaflet segments are often thin and translucent, and of normal height. The posterior annulus may be dilated, but the size of the anterior leaflet and valve are most often normal.
Type I dysfunction with normal leaflet motion and pure annular dilatation is a less common form of degenerative valve disease. It may be associated with conditions that result in significant atrial dilatation such as long-standing atrial fibrillation, or may occur in patients with connective tissue disorders.
* Modified from Carpentier A, Adams DH, Filsoufi F. Carpentier’s Reconstructive Valve Surgery. From Valve Analysis to Valve Reconstruction. 2010 Saunders Elsevier.
Portions excerpted, with permission, Adams DH, Anyanwu AC. The cardiologist's role in increasing the rate of mitral valve repair in degenerative disease. Current Opinion in Cardiology 2008, 23:105-110
- 1Castillo JG, Anyanwu AC, Fuster V, Adams DH. A near 100% repair rate for mitral valve prolapse is achievable in a reference center: implications for future guidelines. J Thorac Cardiovasc Surg. 2012 Aug;144(2):308-12
- 2Castillo JG, Anyanwu AC, El-Eshmawi A, Adams DH. All anterior and bileaflet mitral valve prolapses are repairable in the modern era of reconstructive surgery. Eur J Cardiotharac Surg.. 2014 Jan;45(1):139-45
- 3Carpentier A. Cardiac valve surgery--the "French correction". J Thorac Cardiovasc Surg 1983 September;86(3):323-37.
- 4Barlow JB, Pocock WA. The significance of late systolic murmurs and mid-late systolic clicks. Md State Med J 1963 February;12:76-7.
- 5Carpentier A, Chauvaud S, Fabiani JN et al. Reconstructive surgery of mitral valve incompetence: ten-year appraisal. J Thorac Cardiovasc Surg 1980 March;79(3):338-48.