Making the Diagnosis
Essentially, all degenerative mitral valves are repairable. By matching echocardiographic findings to the appropriate surgical skill level required to consistently deliver a repair, valve replacement for degenerative mitral valve disease should be infrequent.
Most patients with mitral regurgitation remain asymptomatic for long periods of time. The most common presenting signs and symptoms include fatigue, decreased exercise capacity, shortness of breath, and palpitations or supra-ventricular arrhythmias such as atrial fibrillation. Auscultatory examination usually reveals a high-pitched systolic murmur radiating from the apex to the axilla. A holosytolic murmur suggests prolapse simultaneous with ejection typical of chordal rupture, whereas a murmur beginning in mid- or late systole favors billowing or chordal elongation. Radiographic findings may include left atrial and ventricular dilatation and prominent pulmonary vasculature in patients with long standing severe mitral regurgitation. The electrocardiogram may be normal, or show evidence of left atrial enlargement or atrial fibrillation.
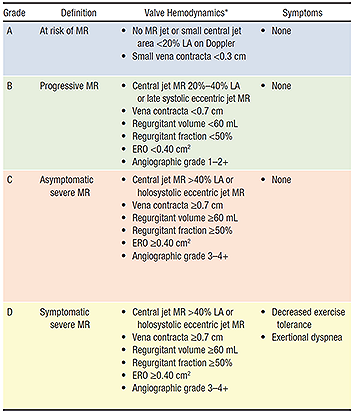
Two-dimensional and Doppler echocardiography is essential to determine the mechanism (dysfunction) and severity of mitral regurgitation. Assessment of the mitral valve hemodynamics using the ratio of jet to left atrial area 1, the regurgitant volume (Rvol: the difference between the mitral and aortic stroke volumes) and effective regurgitant orifice (ERO: ratio of regurgitant volume to regurgitant time velocity integral) are useful tools in grading the severity of MR (Table 12), when integrated with clinical findings. Recent guidelines published by the AHA/ACC joint committee propose a more integrative MR severity grading system ranging from grade A (least severe) to grade C, which defines MR as at risk, progressive, asymptomatic severe and symptomatic severe (Table 2)3
The direction of the jet provides evidence of segmental involvement as it is typically opposite to the prolapsing segment.
Transesophageal echocardiography (TEE) is a useful adjunct to confirm the diagnosis and understand the mechanism of degenerative valve disease in the case of a non-diagnostic transthoracic examination. Experience is also gaining with 3-dimensional echocardiography in the assessment of annular geometry and leaflet dysfunction in the setting of mitral regurgitation, and can be predicted to have a more significant role in planning reparative procedures in the future.
- 1Zoghbi WA, Enriquez-Sarano M, Foster E et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003 July;16(7):777-802.
- 2Dujardin KS, Enriquez-Sarano M, Bailey KR, et al: Grading of mitral regurgitation by quantitative Doppler echocardiography: calibration by left ventricular angiography in routine clinical practice. Circulation 96(10):3409-15 1997.
- 3Nishimura RA et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Circulation. 2014 Jun 10;129(23):e521-643