Fibroelastic Deficiency
In contrast to Barlow’s disease, patients with mitral regurgitation due to fibroelastic deficiency have a lack of connective tissue as the pathological mechanism that triggers leaflet and chordal thinning and eventual chordal rupture1. Carpentier’s group characterized the typical findings in fibroelastic deficiency, noting that the chordal rupture resulting in mitral valve prolapse was often isolated, usually leading to prolapse of a single leaflet segment2.
Clinical Presentation
The typical patient with fibroelastic deficiency is over the age of 60 years, and does not have a long history of a heart murmur. Often asymptomatic until the time of chordal rupture, the patient often presents with palpitations or shortness of breath of limited duration. Patients may remain asymptomatic after chordal rupture, and present as a new-onset murmur or abnormal echocardiogram, but this is less frequent than in the setting of Barlow’s disease. Physical examination is remarkable for a holosystolic murmur, often harsh in nature.
Echocardiographic Findings
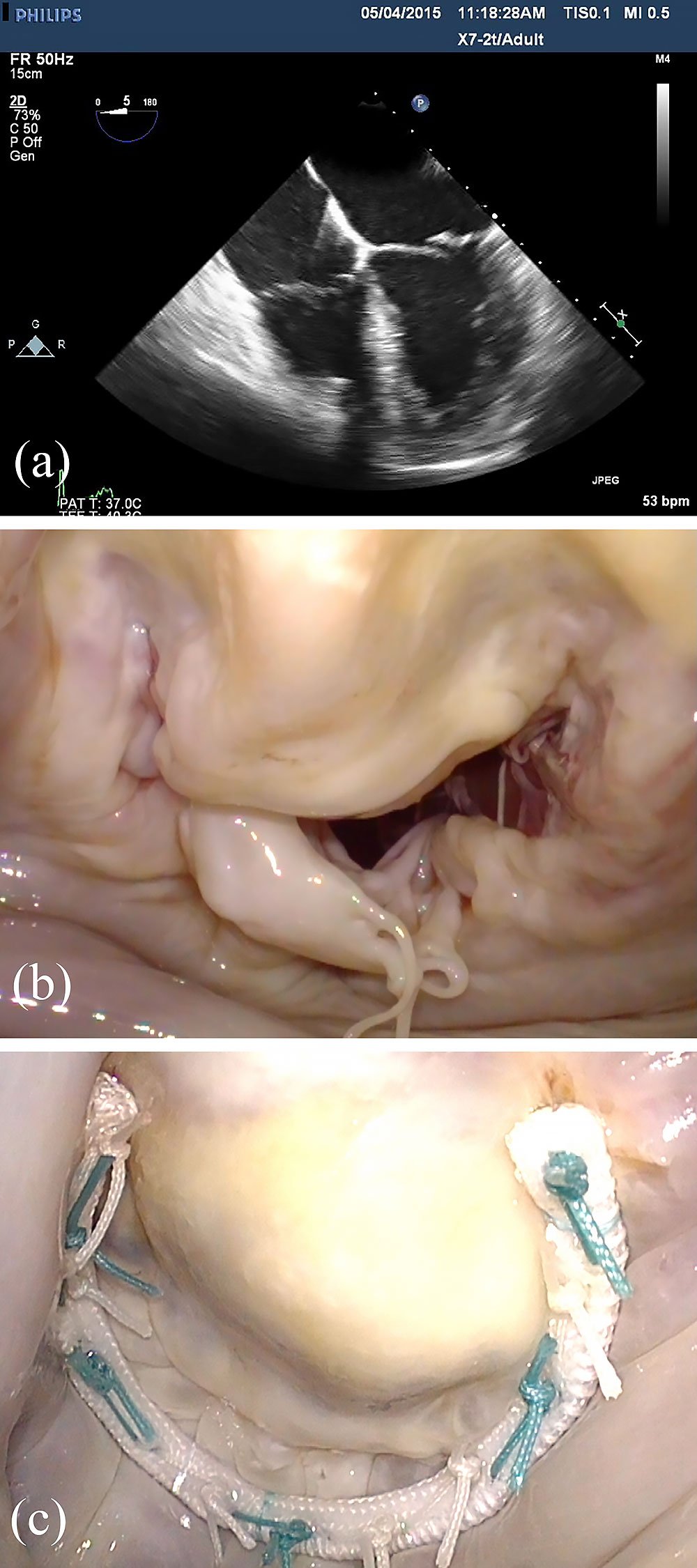
In contrast to Barlow’s disease, echocardiographic signatures of fibroelastic deficiency include normal or near-normal valve size, thin leaflets and chordae, and typically single segment prolapse, most commonly of the middle scallop of the posterior leaflet (P2) (Figure 2). The prolapsing segment may appear to be distended, thickened, and elongated, while the adjacent segments appear normal in height and consistency. Billowing of nonprolapsing segments is not observed, and bi-leaflet dysfunction is uncommon.
Surgical Considerations
In contradistinction to Barlow’s disease, patients with fibroelastic deficiency often present with minimal, as opposed to excess, tissue (Figure 2), so extensive leaflet resection or complex leaflet remodeling procedures are rarely indicated. In general, a limited quadrangular or triangular resection, or simple leaflet resuspension with a chordal transfer or artificial chord, is all that is required to correct leaflet prolapse. For posterior leaflet prolapse, although the prolapsing segment may look very abnormal, the remainder of the valve is relatively unaffected, so that the surgeon does not usually require advanced techniques to achieve a successful mitral valve reconstruction.
It should, however, be noted that “complex” prolapse can occur in fibroelastic deficiency, usually involving an anterior leaflet segment or a commissural segment, and in this setting more advanced techniques and surgical skill are generally required to perform a successful reconstruction. Otherwise, simple fibroelastic deficiency with P2 prolapse is a condition associated with high repair rates in most experienced surgeons’ hands, and a virtually 100% repair rate within a reference center setting with a mitral repair subspecialist3 (Table 1).
- 1 Anyanwu AC, Adams DH. Etiologic Classification of Degenerative Mitral Valve Disease: Barlow's Disease and Fibroelastic Deficiency. Semin Thorac Cardiovasc Surg 2007; 19:90-96.
- 2Carpentier A, Chauvaud S, Fabiani JN, et al. Reconstructive surgery of mitral valve incompetence: ten-year appraisal. J Thorac Cardiovasc Surg 1980; 79:338-348
- 3Castillo JG, Anyanwu AC, Fuster V, Adams DH. A near 100% repair rate for mitral valve prolapse is achievable in a reference center: implications for future guidelines. J Thorac Cardiovasc Surg 144(2):308-12