Leaflets
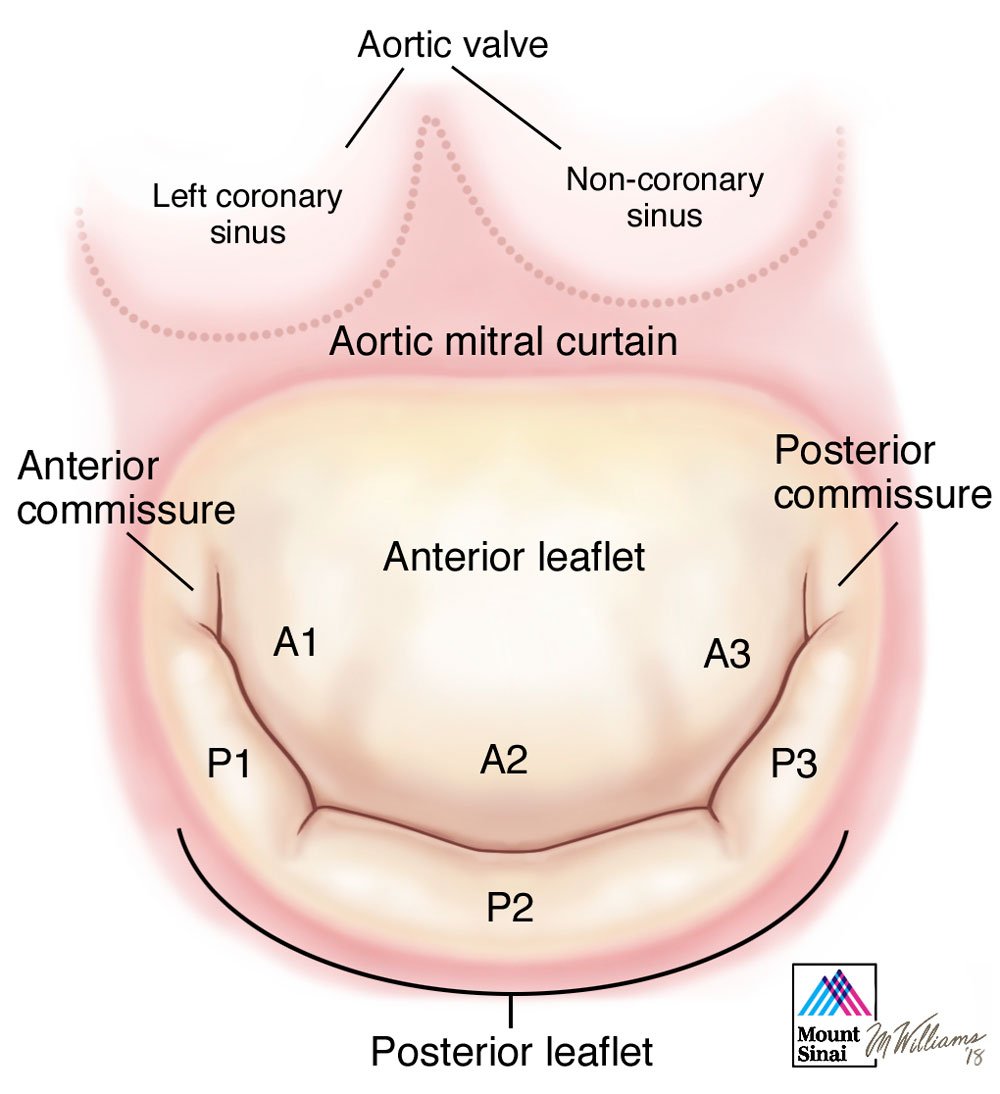
The mitral valve has two leaflets. The anterior leaflet has a semi-circular shape and attaches to two fifths of the annular circumference. There is continuity between the anterior leaflet of the mitral valve and the left and non-coronary cusp of the neighboring aortic valve, referred to as the aortic-mitral curtain. These two components of the aorto-mitral curtain are on two separate anatomical planes, situated at an angle of 120o which corresponds to the planes of the aortic and mitral annulus respectively. The free edge of the anterior leaflet is usually continuous, without indentations. The lack of redundancy of this leaflet along its margin must be taken into consideration in the setting of anterior leaflet prolapse as only small areas of leaflet can be safely resected. The motion of the anterior leaflet also defines an important boundary between the inflow (during diastole) and outflow (during systole) tracts of the left ventricle.
The posterior leaflet of the mitral valve has a quadrangular shape and is attached to approximately three fifths of the annular circumference. The posterior leaflet typically has two well defined indentations which divides the leaflet into three individual scallops identified as P1 (anterior or medial scallop), P2 (middle scallop), and P3 (posterior or lateral scallop). The three corresponding segments of the anterior leaflet are A1 (anterior segment), A2 (middle segment), and A3 (posterior segment)1. This nomenclature is an important tool to describe specific anatomic segmental anatomy between echocardiographer and surgeon. Indentations aid in posterior leaflet opening during diastole. They also imply redundancy to the margin of the posterior leaflet, particularly in the setting of prolapse which triggers a process leading to excess tissue in the prolapsing segment, which therefore allows more aggressive resection compared to the anterior leaflet. The height of the posterior leaflet is less than the anterior leaflet, however, both leaflets have similar surface areas.
* Modified from Carpentier A, Adams DH, Filsoufi F. Carpentier’s Reconstructive Valve Surgery. From Valve Analysis to Valve Reconstruction. 2010 Saunders Elsevier.
- 1Carpentier A. Cardiac valve surgery--the "French correction". J Thorac Cardiovasc Surg 1983 September;86(3):323-37.
Schedule an Appointment or Ask a Question
Who Should Perform Your Surgery?
A given surgeon may have an overall repair rate of 90%, a repair rate of 99% for fibroelastic deficiency with single segment posterior leaflet prolapse due to chordal rupture, but a 25% success rate for Barlow’s disease with bileaflet prolapse. Patients should therefore be considered on an individual basis and for each case the probability of repair for that case by the nominated surgeon (and not a global surgeon or institution repair rate) should be considered.